Welcome to the Research and Strategy Services at in today's fast-paced.


If you’re here because you (or someone you care about) had a fall, a knock, a minor car accident, or a “that didn’t seem that bad… but now I feel weird” moment—this is for you.
A concussion can be confusing precisely because it doesn’t always look dramatic from the outside. You might feel mostly fine at first, then off later. Or you might feel “not myself” in a way that’s hard to put into words. That’s common. Symptoms can also shift over time during recovery.
This guide is a practical 101: how concussions are sustained, what they involve, what to do next, and how to judge when medical care is warranted.
A concussion is a type of mild traumatic brain injury (often shortened to “mTBI”). It happens when a force causes the brain to move rapidly inside the skull—sometimes from a direct blow to the head, but also from hits to the body that whip the head/neck (think: falls, collisions, sudden stops).
What’s helpful to know is this:
One of the most frustrating things about concussions is how individual they are.
Two people can have what looks like the same incident—same fall, same bump—and have very different experiences afterward. Symptoms can be different from person to person, and can also change during recovery.
A few reasons this happens:
A relatable way many people describe it is:
“I’m technically awake and functioning… but my brain feels like it’s running on low battery.”
Sports are one cause, but far from the only one. Many concussions happen in everyday life.
Loss of consciousness is not required.
You can sustain a concussion from a force to the body that causes rapid head/neck motion (like whiplash).
This one is deeply ingrained. The more modern, practical guidance is: sleep is usually okay and often helpful, as long as the person isn’t showing “danger signs” that suggest something more serious. The CDC specifically notes you can let someone sleep uninterrupted after a concussion if there are no danger signs. CDC+1
A good rule of thumb: if the person is worsening, hard to wake, repeatedly vomiting, confused, having a seizure, or showing other red flags, that’s not “go to sleep and see what happens”—that’s urgent medical evaluation.
A normal scan can be reassuring (it helps rule out bleeding or fracture), but concussion symptoms can still be real and significant.
It can help to normalize this: concussions are often sustained during ordinary life events, such as:
For parents: kids can sustain concussions from playground falls, rough housing, and bike/scooter crashes—not just team sports.
Medical lists can feel abstract, so here are symptom categories in “human language.” The CDC summarizes that symptoms can affect how you feel, think, act, or sleep—and that they can evolve over time.
Not everyone follows a neat timeline, but many people find it reassuring to have a general map.
This can be the “what just happened?” stage. Symptoms may be immediate or delayed.
Common experiences: headache, fogginess, nausea, tiredness, needing quiet.
Practical focus:
Many people gradually improve here, though symptoms can fluctuate. For minor head injury/concussion, some sources note symptoms may last up to around 2 weeks.
Common experiences: fatigue, sensitivity to busy environments, trouble focusing at work/school, irritability.
Practical focus:
A smaller subset of people have symptoms that last longer than expected (often referred to as persistent post-concussive symptoms). Mayo Clinic notes that if symptoms persist beyond three months, they may be termed “persistent,” and can sometimes last much longer.
If you’re in this group, it doesn’t mean you’re “broken.” It usually means the systems involved (sleep, vestibular, vision, headache pathways, autonomic stress response) need more targeted support.

If you suspect a concussion, it’s reasonable to seek medical advice—especially for children, older adults, or anyone with complicating factors. The first step is to recognize if there are danger signs that require urgent care.
There’s no single “concussion pill.” Most treatment is symptom-guided and focused on gradual return to normal activity.
Common elements include:
Mayo Clinic’s overview emphasizes evaluation, symptom monitoring, and a staged approach back to activity, with imaging used selectively to rule out more severe injury. Mayo Clinic+1
Usually, yes—if there are no danger signs. The CDC notes it’s okay to let someone sleep uninterrupted after a concussion as long as they aren’t showing danger signs.
A practical approach many families use: check on the person periodically early on to ensure they’re rousable and not worsening, and seek urgent care if anything changes.
No. A force to the body that causes rapid head/neck motion (like whiplash) can be enough.
Yes. Symptoms can appear right away or be delayed, and they can change over the recovery period.
Common symptoms include headache, dizziness, nausea, sensitivity to light/noise, brain fog, trouble concentrating, mood changes, and sleep disruption.
Many people improve within days to weeks, but it varies. Some guidance notes minor concussion symptoms can last up to around two weeks.
If symptoms persist longer, follow-up care is a good idea.
If screens clearly worsen symptoms (headache, nausea, fog), reduce them early on and reintroduce gradually. The goal is to avoid symptom spikes—not to impose total deprivation forever.
Prioritize safety monitoring for red flags, rest, hydration, and a calmer environment. If symptoms are significant, worsening, or the person is high-risk, seek medical advice.
If you’re dizzy, slow to react, foggy, or sensitive to light, driving may be unsafe. When in doubt, avoid driving until you’re clearly steady and/or you’ve been medically advised.
The key practical takeaway is simple: don’t rush back into situations where another head impact could happen until you’ve recovered and been cleared (especially for sport). A second injury before recovery can be dangerous.
Mood changes can be part of concussion physiology (and also a very normal response to feeling “off”). If mood symptoms are intense or persistent, it’s worth discussing with a clinician.
If symptoms are persisting beyond a couple of weeks, worsening, or interfering with normal life, seek follow-up. Some NHS resources advise contacting a GP if symptoms persist beyond a few weeks.
Once you’ve recovered and/or have been medically cleared, many people benefit from a gradual rebuild of physical conditioning, sleep consistency, stress regulation, and cognitive endurance—especially if they’re returning to demanding work, study, or sport.
If you’d like ideas on tech-supported options that can support a functional return to peak performance after concussion recovery, here’s an additional guide: Top Tech Tools for Functional Return to Peak Performance After Concussion Recovery







Welcome to the Research and Strategy Services at in today's fast-paced.

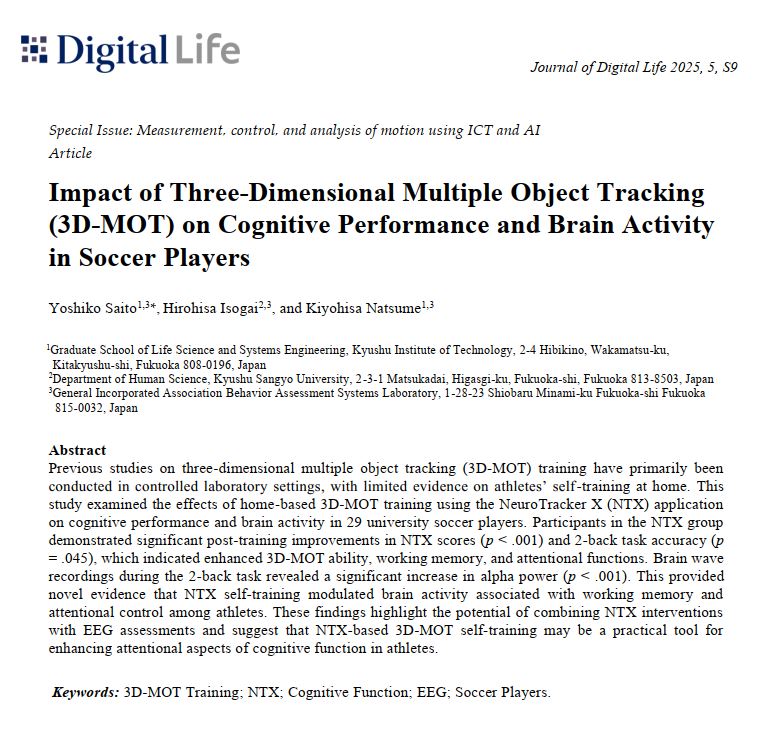
Rest can help cognitive recovery, but focus doesn’t always return immediately. This article explains why different cognitive systems recover at different speeds and why improvement often unfolds gradually.

Cognitive recovery is rarely linear — and improvement doesn’t always look immediate. This guide explains how recovery unfolds over time and why sustainability depends on recalibration, not quick resets.

Cognitive scores naturally fluctuate — but patterns matter more than single sessions. This guide explains how to distinguish noise from meaningful change over time.
.png)